妊娠糖尿病产后早期血脂下降率与糖代谢异常的相关性分析
作者: 李亚俐
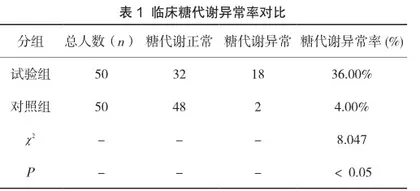
【摘要】目的:观察分析妊娠糖尿病产后早期血脂下降率与糖代谢异常的相关性。方法:对医院在2019年1月—2020年12月收治的100例妊娠糖尿病患者作为研究对象,根据其孕期血脂异常情况进行分组,对照组为血脂正常的妊娠糖尿病患者(n=50),试验组为血脂水平异常妊娠糖尿病患者(n=50),对比两组患者产后早期血脂、糖代谢参数变化。结果:对比两组患者糖代谢异常患者比例,对照组糖代谢异常患者比例36.00%,试验组4.00%,两组比较有统计学意义(P<0.05)。对比两组患者产后早期血脂水平下降情况、糖代谢参数变化,试验组患者产后总胆固醇TC、甘油三酯TG、高密度脂蛋白胆固醇HDL-C水平、空腹血糖FPG、孕期糖负荷1h血糖水平变化,与对照组比较存在差异,有统计学意义(P<0.05)。相关性分析中,TG、TG/HDL-C与产后糖代谢异常呈正相关,HDL-C与产后糖代谢异常呈负相关(P<0.05)。结论:在临床对妊娠糖尿病产后早期血脂下降患者,早期血脂下降率与糖代谢异常具有相关性,可通过调节其血脂下降异常水平,以规避糖代谢异常风险,提升患者临床疗效,可在实践中推广应用。
【关键词】妊娠糖尿病;糖代谢异常;血脂水平;产后
Analysis of the correlation between the rate of lipid decline and abnormal glucose metabolism in the early postpartum period of pregnancy with diabetes
LI Yali
Baoji Third Hospital, Baoji, Shaanxi 721004, China
【Abstract】Objective: To observe and analyze the correlation between the rate of blood lipid decline in the early postpartum period of pregnancy with diabetes and abnormal glucose metabolism. Methods: 100 patients with gestational diabetes admitted by the hospital from January 2019 to December 2020 were taken as the research object, and were divided into groups according to their abnormal blood lipids during pregnancy. The control group was pregnant diabetes patients with normal blood lipids (n=50), and the test group was pregnant diabetes patients with abnormal blood lipids (n=50). The changes of blood lipids and glucose metabolism parameters in the early postpartum period were compared between the two groups. Results: The proportion of patients with abnormal glucose metabolism was compared between the two groups. The proportion of patients with abnormal glucose metabolism in the control group was 36.00%, while that in the test group was 4.00%. There was statistical significance between the two groups(P<0.05). The decrease of blood lipid level and changes of glucose metabolism parameters in the early postpartum period were compared between the two groups. The changes of total cholesterol (TC), triglyceride (TG), highdensity lipoprotein cholesterol (HDL-C), fasting blood glucose (FPG), and blood glucose level in pregnancy in the test group were statistically significant compared with the control group (P<0.05). In the correlation analysis, TG, TG/HDL-C were positively correlated with abnormal postnatal glucose metabolism, while HDL-C was negatively correlated with abnormal postnatal glucose metabolism (P<0.05). Conclusion: In clinical practice, for patients with pregnancy diabetes and early postpartum blood lipid decline, the rate of early blood lipid decline is related to abnormal glucose metabolism. The abnormal level of blood lipid decline can be adjusted to avoid the risk of abnormal glucose metabolism, improve the clinical efficacy of patients, and can be popularized in practice.